ABCGN Certified Gastroenterology Registered Nurse Exam Braindumps
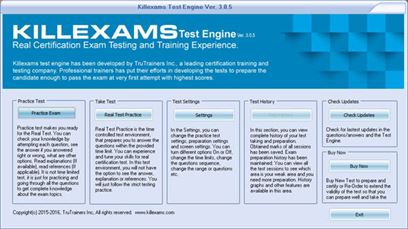
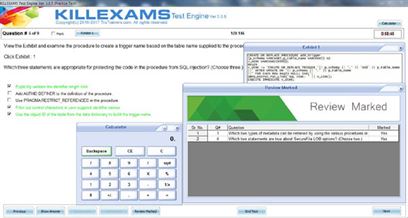
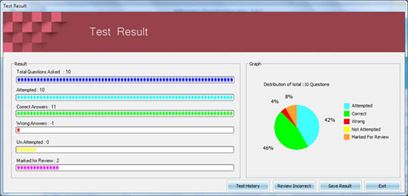
Killexams.com CGRN Exam Braindumps contain complete question pool, updated in April 2024 including VCE exam simulator that will help you get high marks in the exam. All these CGRN exam questions are verified by killexams certified professionals and backed by 100% money back guarantee.
CGRN approach - ABCGN Certified Gastroenterology Registered Nurse Updated: 2024 | ||||||||
| Don't Miss these CGRN CGRN Dumps | ||||||||
 |
||||||||
|
||||||||
|
Exam Code: CGRN ABCGN Certified Gastroenterology Registered Nurse approach January 2024 by Killexams.com team | ||||||||
CGRN ABCGN Certified Gastroenterology Registered Nurse The Examination: There is one ABCGN certification examination for RNs. The examination is based on role delineations -- surveys of practitioners, which define the scope of practice and the knowledge and skills required to function in the field. All examination items are written by certified individuals with expertise in the field of gastroenterology and/or gastroenterology endoscopy nursing practice. Test Items (Questions): Test items are reviewed, referenced and validated by the ABCGN Item Writers Committee and, finally, edited by the testing company for construction, grammatical correctness and clarity. Examination Content The CGRN examination each consist of 175 multiple-choice questions. Each question has four choices and one correct answer. Candidates have three hours to complete their examination. The CGRN examination contains questions from four major content areas: general nursing care, gastroenterological procedures, patient care interventions and environmental safety, infection prevention and control. All questions are directly related to the GI specialty. More specific information regarding the content of the examinations is included in the Appendix of the Certification Handbook. Preparation for the Examination: ABCGN does not sponsor or endorse test preparation or review courses for the certification examinations. SGNA, ABCGN's sister organization, offers both courses and materials for the test and recertification. Visit the SGNA website for more details. 1. General Nursing Care 24% 2. Gastroenterological Procedures 33% 3. Patient Care Interventions 27% 4. Environmental Safety, Infection Prevention and Control 16% Domain I: General Nursing Care Task A: Assess and analyze the patients health status through data collection. Knowledge of: 1. Normal and abnormal gastrointestinal anatomy, physiology, and pathophysiology 2. Physiological, psychological, social, cultural, and spiritual aspects of their wellness 3. Pharmacology (e.g. Prescription medication, OTC, supplements-herbal) Task B: Monitor and assess the patients health status to determine necessary nursing interventions. Knowledge of: Normal and abnormal gastrointestinal anatomy, physiology, and pathophysiology 2. Physiological, psychological, social, cultural, and spiritual aspects of their wellness 3. Pharmacology (e.g. compliance/noncompliance issues, education, drug interaction) 4. Advocating and protecting patients rights and privacy (e.g. HIPAA, ethics) Task C: Educate the patient through effective communication to develop a plan of care directed to the patients level of understanding. Knowledge of: 1. Normal and abnormal gastrointestinal anatomy, physiology, and pathophysiology 2. Physiological, psychological, social, cultural, and spiritual aspects of their wellness 3. Pharmacology (e.g. Prescription medication, OTC, supplements-herbal) Domain II: Gastroenterological Procedures Task A: Collaborate with the health care team during endoscopic procedures to provide safe and effective care. Knowledge of: 1. Endoscopic procedures ( e.g. diagnostic, interventional) 2. Equipment and accessories 3. Normal and abnormal gastrointestinal anatomy, physiology, and pathophysiology 4. Environment of care (e.g. thermal burns, chemical spills, radiation, time out) 5. Pharmacology(e.g. sedation medication, reversal agents, procedure medications, resuscitative medication) 6. Physiological, psychological, social, spiritual, and cultural aspects of wellness 7. Potential complications and anticipated interventions (e.g. hemorrhage, perforation, compromised airway, medication reaction) 8. Specimen processing and handling (e.g. labeling, storage, transportation) Task B: Collaboration with the health care teamduring non-endoscopic procedures to provide safe and effective care. Knowledge of: 1. Non-endoscopic procedures (e.g. diagnostic, interventional) 2. Equipment and accessories (e.g. needles, probes, capsules, ligature, PEG exchange) 3. Normal and abnormal gastrointestinal anatomy, physiology, and pathophysiology 4. Environment of care (e.g. spills, time out) 5. Pharmacology(e.g. learning needs, sedation medication, reversal agents, procedure medications, resuscitative medication) 6. Physiological, psychological, social, spiritual, and cultural aspects of wellness 7. Potential risks, complications, and interventions 8. Specimen processing and handling (e.g. labeling, storage, transportation) Task C: Perform non-endoscopic procedures to promote optimal patient outcomes. Knowledge of: 1. Non-endoscopic procedures (e.g. diagnostic, interventional) 2. Equipment and accessories (e.g. probes, capsules, PEG exchange) 3. Normal and abnormal gastrointestinal anatomy, physiology, and pathophysiology 4. Environment of care (e.g. time out, spills) 5. Pharmacology (e.g. biologics) 6. Physiological, psychological, social, spiritual, and cultural aspects of wellness 7. Potential risks, complications, and interventions 8. Specimen processing and handling (e.g. labeling, storage, transportation) Domain III: Patient Care Interventions Task A: Recognize and respond to emergent changes in the patients status to prevent complications and maximize positive outcomes. Knowledge of: 1. Potential risks, complications, and anticipated interventions (e.g. underlines conditions) 2. Resuscitation procedures and equipment 3. Normal and abnormal gastrointestinal anatomy, physiology, and pathophysiology 4. Emergency medications (e.g. Romazicon, Atropine, Narcan, Epinephrine) 5. Sedation guidelines and principles (e.g. ASA, airway status) Task 2: Promoting wellness by managing GI health care needs. Knowledge of: 1. Diet and Nutrition (e.g. supplements, high fiber diet, other specialized diets, diet modifications) 2. Normal and abnormal gastrointestinal anatomy, physiology, and pathophysiology 3. Therapeutic interventions in pain management (e.g. ambulation, medication, positioning) 4. Patients rights and responsibilities (e.g. advanced directives) 5. Pharmacology (e.g. PPI, laxative, pro-biotics, biologics, timing of medication) 6. Potential complications (e.g. flare ups, drug reactions/interactions) 7. Physiological, psychological, social, sexual, spiritual, and cultural aspects of wellness 8. Resources (e.g. palliative, support group, financial and social assistance) Task C: Administer medications and fluids consistent to provide safe and effective care. Knowledge of: 1. Established standards for administering medications and fluids (e.g. safe injection practices) 2. Normal and abnormal gastrointestinal anatomy, physiology, and pathophysiology 3. Pharmacology (e.g. biologics infusions/injections, antibiotic, timing of medication) 4. Physiological, psychological, social, cultural, and spiritual aspects of wellness 5. Potential adverse reactions, complications, and anticipated interventions Domain IV: Environmental Safety, Infection Prevention and Control Task A: Procedure related infection prevention and control. Knowledge of: 1. Standard for infection control in an endoscopy setting (e.g. validation of competencies, manufactures guidelines, PPE, spills) 2. Equipment reprocessing (e.g. Scopes and accessories, bioburden) 3. Sterilization and high level disinfection (e.g. Spaulding classification, single use devices vs. reusable devices, minimal effective concentration of disinfection solutions 4. Safe Injection practices (e.g. multi-dose vial) 5. Body mechanics (e.g. ergonomics, patient pressure, repetitive injuries) 6. Electrical, Laser, Radiation, Chemical (e.g. grounding pad placement, piercings, return electrode) Task B: Environmental Safety, Infection Prevention and Control in Gastroenterology Knowledge of: 1. Patient education related to disease (e.g. Crohns, C-DIFF, VRE, CRE) 2. Bloodborne pathogen (e.g. Hepatitis C, transmission) 3. Multidrug resistance organisms (e.g. MDRO, VRE, CRE) 4. Personal Protective Equipment (e.g. standard precautions, communication devices, attire) | ||||||||
| ABCGN Certified Gastroenterology Registered Nurse Medical Gastroenterology approach | ||||||||
Other Medical examsCRRN Certified Rehabilitation Registered NurseCCRN Critical Care Register Nurse CEN Certified Emergency Nurse CFRN Certified Flight Registered Nurse CGFNS Commission on Graduates of Foreign Nursing Schools CNA Certified Nurse Assistant CNN Certified Nephrology Nurse CNOR Certified Nurse Operating Room DANB Dental Assisting National Board Dietitian Dietitian EMT Emergency Medical Technician EPPP Examination for Professional Practice of Psychology FPGEE Foreign Pharmacy Graduate Equivalency NBCOT National Board for Certification of Occupational Therapists - 2023 NCBTMB National Certification Board for Therapeutic Massage & Bodywork NET Nurse Entrance Test NPTE National Physical Therapy Examination OCN Oncology Certified Nurse - 2023 PANCE Physician Assistant National Certifying VTNE Veterinary Technician National Examination (VTNE) CNS Clinical Nurse Specialist NBRC The National Board for Respiratory Care AHM-540 AHM Medical Management AACN-CMC Cardiac Medicine Subspecialty Certification AAMA-CMA AAMA Certified Medical Assistant ABEM-EMC ABEM Emergency Medicine Certificate ACNP AG - Acute Care Nurse Practitioner AEMT NREMT Advanced Emergency Medical Technician AHIMA-CCS Certified Coding Specialist (CPC) (ICD-10-CM) ANCC-CVNC ANCC (RN-BC) Cardiac-Vascular Nursing ANCC-MSN ANCC (RN-BC) Medical-Surgical Nursing ANP-BC ANCC Adult Nurse Practitioner APMLE Podiatry and Medical BCNS-CNS Board Certified Nutrition Specialis BMAT Biomedical Admissions Test CCN CNCB Certified Clinical Nutritionist CCP Certificate in Child Psychology CDCA-ADEX Dental Hygiene CDM Certified Dietary Manager CGRN ABCGN Certified Gastroenterology Registered Nurse CNSC NBNSC Certified Nutrition Support Clinician COMLEX-USA Osteopathic Physician CPM Certified Professional Midwife CRNE Canadian Registered Nurse Examination CVPM Certificate of Veterinary Practice Management DAT Dental Admission Test DHORT Discover Health Occupations Readiness Test DTR Dietetic Technician Registered FNS Fitness Nutrition Specialist MHAP MHA Phlebotomist MSNCB MSNCB Medical-Surgical Nursing Certification NAPLEX North American Pharmacist Licensure Examination NCCT-TSC NCCT Technician in Surgery NCMA-CMA Certified Medical Assistant NCPT National Certified Phlebotomy Technician (NCPT) NE-BC ANCC Nurse Executive Certification NNAAP-NA NNAAP Nurse Aide NREMT-NRP NREMT National Registered Paramedic NREMT-PTE NREMT Paramedic Trauma Exam OCS Ophthalmic Coding Specialist PANRE Physician Assistant National Recertifying Exam PCCN AACN Progressive Critical Care Nursing RDN Registered Dietitian VACC VACC Vascular Access WHNP Women Health Nurse Practitioner AACD American Academy of Cosmetic Dentistry RPFT Registered Pulmonary Function Technologist ACLS Advanced Cardiac Life Support - 2023 GP-Doctor General Practitioner (GP) Doctor GP-MCQS Prometric MCQS for general practitioner (GP) Doctor INBDE Integrated National Board Dental Examination (Day 1 exam) Podiatry-License-Exam-Part-III Podiatry License test Part III - 2023 | ||||||||
| killexams.com CGRN test study guides are setup by our IT professionals. Killexams.com experts work out this comprehensive version of CGRN dumps contain real test questions and answers. Everything is to make convenience for candidates on their road to certification. Memorizing these CGRN dumps and practice questions and forget to fail the exam. | ||||||||
| Medical CGRN ABCGN Certified Gastroenterology Registered Nurse https://killexams.com/pass4sure/exam-detail/CGRN Question: 49 When draining a client's ileostomy bag and changing the dressings, the nurse should use which of the following protective measures? A. Sterile gloves, sterile mask, gown B. Double gloves, goggles, mask, gown C. Goggles, gown, booties and mask D. Sterile and clean gloves, mask, gown Answer: D Standard precautions needed when caring for an ileostomy include clean gloves, mask, and gown when draining the bag, and a sterile glove when changing the dressing. The nurse should change gloves in between the two procedures to avoid contact with body fluids. Goggles are used if the procedure would likely generate a splash or spray of body fluids. Question: 50 50. A nurse is assigned to a 25-year-old woman scheduled for therapeutic termination of pregnancy due to a recently discovered heart condition of the mother. The nurse refuses to care for this client because of a conflict in religious beliefs. How should the charge nurse handle this situation? A. Insist that the nurse accept the delegated task. B. Ask the nurse to set aside her beliefs for the sake of nursing care. C. Assign the nurse to another client. D. Ask the nurse to document her refusal in the client's chart. Answer: C The charge nurse or the employer should certain free exercise of beliefs without discrimination. Some nurses have religious beliefs that may prohibit them from participating in certain procedures. Employers should accommodate the nurse's request not to participate in any care or procedure that is in conflict with their religious beliefs. A written statement should be provided by the nurse indicating the moral or religious basis for refusing the client assignment. Question: 51 A patient diagnosed with a peptic ulcer is prescribed with sucralfate. Which of the following instructions should be given to the patient to ensure that the medication is taken appropriately? A. Sucralfate is taken with meals B. Sucralfate should be administered together with an antacid C. Sucralfate should be administered two hours apart from warfarin sodium D. Sucralfate can cause diarrhea; increased fiber intake is recommended Answer: C Sucralfate may impede the absorption of warfarin sodium, phenytoin, theophylline, and digoxin. These medications should be administered at least two hours apart from each other. Sucralfate should be administered on an empty stomach and at least 60 minutes apart from an antacid. Constipation is a common side effect of sucralfate. Question: 52 A client has a serum calcium level of 5.0 mg/dL. As the nurse reviews the client's records, which information is the most likely cause of the laboratory result? A. Over activity of parathyroid glands B. Excessive vitamin D levels C. Intake of furosemide D. Renal failure Answer: C The normal serum calcium level is between 8.6 and 10.0 mg/dL. A calcium level of 5.0 mg/dL indicates hypocalcemia. Loop diuretics, such as furosemide, may increase the excretion of calcium, which increases the risk for hypocalcemia. The other options increase the risk for hypercalcemia. Question: 53 A patient diagnosed with hepatic encephalopathy is prescribed with lactulose. The medication treats liver cirrhosis by the following actions except: A. It decreases the pH of the bowel B. It decreases ammonia production by the bacteria C. It promotes ammonia excretion. D. It reduces the number of colonic bacteria that convert urea and amino acids into ammonia. Answer: D Lactulose decreases ammonia levels, improves protein tolerance, and lowers colonic pH that results in ammonia excretion. Neomycin is used to reduce the number of colonic bacteria that produces ammonia. Question: 54 A nurse is assigned in the triage area of the emergency department. The nurse is assigned to care for a three-year-old child complaining of severe abdominal pain. Further assessment shows abdominal distension, shortness of breath, and lethargy. What is the appropriate category for this child? A. Red B. Green C. Yellow D. Black Answer: A This child's condition is categorized as RED, which requires the highest priority. This category is given to patients with life-threatening conditions, such as airway obstruction, decreased level of consciousness, and massive or uncontrolled bleeding. The GREEN category has the lowest priority. YELLOW is reserved for clients with serious but not life-threatening conditions. The BLACK category is given to deceased or non-salvageable clients. Question: 55 Which of the following best describes the recommended diet for the client with Meniere's syndrome? A. High in fiber B. Low in sodium C. High in iodine D. Low in fiber Answer: B A low-sodium diet is best for the client with Meniere's syndrome. Question: 56 A client who had just undergone hemodialysis is ordered for a laboratory test. Which of the following parameters will show a significant improvement after dialysis? A. Creatinine B. Hemoglobin C. Phosphorus D. Calcium Answer: A The best indicator of client's response to dialysis is a decrease in creatinine level. Creatinine is used to measure how well the kidneys can filter fluids. On the other hand, dialysis will result in diminishing hemoglobin level (renal anemia), increased phosphorus and decreased calcium which are all part of disease process of CKD. Question: 57 An RN delegates some tasks to the LPN. The RN's first consideration when delegating tasks is which of the following? A. Client ratio during the shift B. Stability of the client's status C. The LPN's familiarity with the skills required D. The LPN's skill level Answer: B The stability of the client's condition would be the nurse's priority when delegating tasks. RNs have to be directly involved in monitoring and giving care if the client is unstable. For More exams visit https://killexams.com/vendors-exam-list Kill your test at First Attempt....Guaranteed! | ||||||||
Oral Bile-Acid TreatmentSuccessful dissolution of gallstones by the oral administration of bile-acid mixtures was reported almost 70 years ago.[22] It was, however, only in the 1970s that this form of therapy was tested on a larger scale.[23,24,25] Initially, CDCA was used,[26] but due to a dose-dependent increase in aminotransferases, an increase in serum low-density lipoprotein cholesterol, and the development of bile salt-induced diarrhea, the treatment raised concerns. Because the more hydrophilic UDCA appeared to be as effective in gallstone dissolution but was practically devoid of side effects, it rapidly replaced the use of CDCA.[27,28] The idea behind oral administration of CDCA and UDCA was to enrich the bile with these bile acids and thereby decrease cholesterol supersaturation and dissolve the stones. In fact, total bile salt concentration in bile did not change appreciably, and the decrease in cholesterol saturation was achieved primarily by a decrease in biliary cholesterol concentration. While both bile acids do decrease biliary cholesterol secretion,[29] they do so by different mechanisms. CDCA decreases cholesterol synthesis by inhibiting hepatic HMG-CoA reductase activity, whereas UDCA does not affect cholesterol synthesis but reduces intestinal cholesterol absorption.[30] CDCA also decreases hepatic bile-acid synthesis, but UDCA does not, and may even slightly increase it. There is also a difference between the 2 agents in terms of the physical chemical mechanism of gallstone dissolution: CDCA removes cholesterol from the stones by micellar solubilization, whereas UDCA does so primarily by formation of a liquid crystalline phase.[31,32] In 1981, the National Cooperative Gallstone Study established the efficacy and safety of CDCA therapy.[26] Although gallstones could be dissolved by oral administration of CDCA, its efficacy was low. Less than half (40.8%) of patients responded to the highest dose tested (750 mg/day), and only 13.5% had complete dissolution of their stones within 2 years. Moreover, the response was slow. In over half, more than 9 months of treatment were needed for complete dissolution. Subsequently, the introduction of UDCA with a better safety profile and equal or better efficacy made bile salt litholysis more attractive. The efficacy of CDCA is dose-dependent, but so are its side effects. Hence, a full dose of 15 mg/kg/day will induce diarrhea in up to 60% of patients, increase cholesterol levels in most patients, and cause hepatotoxicity in over 3%. In comparison, the recommended dose of UDCA (10-12 mg/kg/day) has essentially no side effects except occasional diarrhea. Therefore, monotherapy with CDCA cannot be recommended and has been completely replaced by UDCA therapy. Combination therapy with a reduced dose of both bile acids (5-8 mg/kg/day of each) has also been suggested, and may be as safe and efficient as full-dose UDCA monotherapy, as well as less costly.[33,34] UDCA monotherapy does, however, cause less diarrhea, and therefore it remains the treatment of choice today. UDCA is usually given at a dose ranging between 8 and 15 mg/kg/day. Bedtime administration is preferable because it maintains hepatic bile-acid secretion rate overnight, thus reducing secretion of supersaturated bile and increasing the dissolution rate.[35,36] Dissolution is assessed by ultrasonography every 6 months. The expected dissolution rate is approximately a 1-mm decrease in stone diameter per month of treatment.[37] Treatment is usually continued for another 3 months after successful dissolution. In up to 10% of patients, cholesterol gallstones acquire a surface calcification during treatment, rendering them nondissolvable and unsuitable for further therapy with bile acids.[38] Not all patients are suitable candidates for oral dissolution therapy. Selection criteria are based on 3 main aspects: (1) patient, (2) gallbladder, and (3) stone characteristics. Patients with complications or with frequent and severe attacks of biliary colic are not suitable candidates. Patients with mildly symptomatic gallstones are the best candidates.[28,39] Patients with increased surgical risks or those who do not want to undergo surgery due to personal preferences should be considered for medical dissolution therapy. Asymptomatic patients are currently not treated. For medical therapy to be effective, the gallbladder needs to fill and function. Finally, only cholesterol stones can be dissolved by bile acids, and any significant calcification of the stones will render them nondissolvable. Gallbladder function -- as well as cholesterol content of stones -- can be assessed by oral cholecystography.[40] After oral intake of an iopanoic acid derivative, a plain abdominal x-ray will show radiolucent cholesterol stones floating within a radiopaque contrast-filled gallbladder.[41] Gallbladder function can be further evaluated by measuring the emptying or ejection fraction following a fatty meal. Ultrasonography is the easiest and most precise method for detecting the presence of stones. Ultrasonography as well as cholescintigraphy may also be used to assess cystic duct patency and gallbladder function by measuring the ejection fraction after a fatty meal or cholecystokinin injection.[42,43,44] Some clinicians have even suggested that ultrasonography may predict stone composition prior to bile-acid or shock-wave lithotripsy treatment.[45,46] Several investigators have shown that the degree of stone calcification and suitability for bile-acid dissolution therapy can be accurately assessed by computed tomography (CT).[47,48,49] Hence, a combination of CT for stone composition and ultrasonography for gallbladder filling and function is also a good alternative for appropriate patient selection. The success of oral dissolution treatment is defined as complete disappearance of gallstones as documented by oral cholecystography or, preferably, ultrasonography. This is achieved in 10% to over 80% of patients. The wide range of success reflects differences in patient selection, treatment duration, dosage, and ways of assessing success.[50] In a meta-analysis comprising almost 2000 patients treated until 1992, complete dissolution was achieved in 18.2% with CDCA, in 37.3% with UDCA, and in 62.8% with combination therapy.[51] In patients with small stones (< 10 mm), a dissolution rate of 48.5% was seen with UDCA therapy. By employing more strict selection criteria, the efficacy of this treatment can be increased, but at the expense of the number of suitable candidates.[52] Thus, an optimal lean patient with small (< 5 mm) radiolucent stones (approximately 3% of all symptomatic patients) will have a 90% likelihood of complete dissolution within 6 months.[53] In contrast, patients with 5- to 10-mm radiolucent stones (approximately 12%) will have only a 50% chance of successful dissolution within 9 months. Initially, extracorporeal shock-wave lithotripsy (ESWL) was introduced as an adjunct to bile-acid therapy.[54,55] The rationale was to use ESWL to fragment larger stones to increase dissolvable surface area, shorten treatment time, and increase the pool of patients suitable for bile-acid dissolution. With increasing experience it became clear that ESWL was actually an independent treatment modality.[56] After pulverizing gallstones to tiny sand-like fragments, there seems to be little if any benefit of or need for additional bile-acid therapy.[56,57,58] A significant drawback of gallstone dissolution therapy is the possibility of gallstone recurrence. Stones will recur because the gallbladder is left in place and the underlying cause of gallstone formation has not been corrected. The recurrence rate is about 10% annually for up to 5 years,[59] and is often preceded by sludge formation.[60] Thereafter, recurrence is uncommon. Most stones recur without symptoms[50] and will respond to re-treatment with bile acids.[61,62] Maintenance therapy with low-dose UDCA has been reported to decrease the recurrence rate but it is costly.[63] Patients with multiple primary stones have an increased recurrence rate.[63] Additional factors that have been reported to predict recurrence after successful lithotripsy are obesity,[64] poor gallbladder emptying,[65] an increased deoxycholic acid pool,[66] and an apoE4 genotype.[67] Whether these factors are important after medical dissolution is unclear. Because successful dissolution therapy is not inevitably followed by gallstone recurrence, there is a group of patients in whom the initial lithogenic process is transient. Pregnancy, rapid weight loss, and convalescence from abdominal surgery are recognized transient risk factors.[68,69] Trying to identify and characterize patients with transient lithogenicity for dissolution therapy is an important challenge for future studies. Gastroenterology and Hepatology TrainingDuring the program, fellows receive training in the cognitive aspects of consultative gastroenterology and hepatology, in gastrointestinal endoscopy and liver biopsies, and have research opportunities. Fellows also have an opportunity to spend six months in laboratory-based or clinical research. An amalgamation of these clinical, procedural and research experiences provides the foundation for a career in academic medicine and scholarly clinical practice. The role of the gastrointestinal specialist has been modified with the changes in health care delivery and the advent of managed care. We are cognizant of these changes and have designed our program to be sufficiently flexible to meet our trainees' needs and allow for future success. This includes creating the dual-pathway training option where a trainee will be board-eligible in both gastroenterology and transplant hepatology in only three years. Complex problems in gastroenterology often require a team approach. We have excellent collaborative relations with GI and liver transplant surgeons, diagnostic and therapeutic radiologists, and GI pathologists who regularly interact with us in our patients' care and research efforts. As a result of this team approach, we are proud to offer the newly ACGME-approved dual-pathway training in our fellowship. This is an exciting opportunity for those interested in being board-eligible in gastroenterology and transplant hepatology. This combined program is designed to be completed in three years rather than as separate programs spanning four years. Saint Louis University has an active abdominal transplantation program. A Supportive Environment
Our teaching hospitals provide fellows with experience treating both common medical conditions seen in community settings and complex cases treated at a major academic tertiary care referral center. Our teaching faculty is an enthusiastic and skilled group of educators, including many who are listed on St. Louis's Best Doctors List. Our faculty and staff are known to be approachable, friendly, and supportive. Fellows are regularly instructed at the bedside by dedicated clinical educators who provide a truly diverse and varied experience. Fellows develop excellent clinical and patient management skills that allow them to become outstanding physicians in any environment. The program fosters self-governance and ownership of the educational experience by the fellows, encouraging self-directed, lifelong learning. Fellowship Clinical Services
During the first year of training, fellows rotate on the gastroenterology service at SSM Health Saint Louis University Hospital and John J. Cochran Veterans Hospital. Fellows become proficient in basic endoscopic procedures. Here is a yearly breakdown: First Year
Second and Third Year
If a trainee is interested in completing the dual-pathway for gastroenterology and transplant hepatology, they may apply in their first year to begin on the adjusted pathway during their second year. These trainees will have the same robust gastroenterology experiences with the following transplant hepatology-specific experiences:
Elective Options
Fellowship Research
Each fellow is expected to complete a research project of clinical or basic science interest. The goal of the research component of the fellowship is to train physicians and basic scientists who want to pursue a career in academic medicine. The program develops independence under the direction of a mentor. A major emphasis of the experience is teaching the skills necessary to perform research and win peer-reviewed funding in our current competitive climate. The research process includes experience in literature review, study design, budgeting, peer review, IRB approval, data collection, statistical analysis, and submission of an abstract for society presentation and publication in a peer-reviewed journal. In addition to the support of the teaching faculty, the fellowship program provides research support consisting of clinical research assistants, computer programming for data analysis, and graphics and audio/visual support for presentations. Each fellow must also present their research at our annual year-end research conferences. Fellows are also encouraged to present the results of their research experiences at an annual national meeting, such as those sponsored by the American Gastroenterological Association, the American Association for the Study of Liver Diseases or the American College of Gastroenterology. Current research activities include:
Training GoalsThe goal of training in the second and third years is for fellows to develop specific skills in keeping with their career goals. Someone interested in general gastroenterology practice might be involved in all clinical areas. Someone interested in a research-oriented academic career would place an emphasis on research. And subspecialty residents interested in a career in academic clinical hepatology might do extensive work in the liver clinic, with the liver transplant service, and with several clinical research projects. The flexibility of the curriculum in the second and third years allows our fellows to tailor their training according to their career choices. Transplant HepatologyOur ACGME-accredited transplant hepatology fellowship is designed for trainees who have already completed their gastroenterology training. Building on the prior training allows this one-year fellowship to deepen the trainee’s knowledge while challenging them with additional skills and procedures. Our program aims to create well-rounded gastroenterologists capable of meeting 21st-century needs in a collaborative approach with their patients, other services and the medical system. If you have any questions, please reach out and let us know. Clinical Research FellowshipBeginning in the 2023-2024 academic year, the Division of Gastroenterology and Hepatology at Saint Louis University will offer a one-year, non-ACGME Clinical Research Fellowship. This full-time, exempt position will report to and work closely with Division Director Wing-Kin Syn, M.D. This is a bespoke one-year clinical research fellowship with potential for extension, focusing on NAFLD with a mixture of research and clinical training. The breakdown will be as follows:
It will suit trainees or junior faculty intending a career as a GI/hepatology physician-researcher or physician-scientist. This blended research and clinical practice fellowship is designed to marry the clinical and research components of the field to enhance patient care. For more information, please contact: Application ProcessYou may apply for one of our four GI fellowship positions through the Electronic Residency Application Service (ERAS). We accept applications July 1-31 for each interview season. We review applications in early August and invite applicants to interview from late August to October. Our positions will be filled through the National Residency Match Program (NRMP). We sponsor both H-1B1 and J-1 visas. All application requirements are listed with ERAS. ResearchThe Division of Gastroenterology and Hepatology at Saint Louis University fosters research from the lab to patient treatment. As a leading research center, we are continually engaged in multicenter clinical trials, allowing us to offer our patients access to the latest advances in clinical care. Our physicians specialize in diagnosing and treating liver diseases that range from the evaluation of fatty liver to hepatitis B to the management of severe, complicated, end-stage liver disease awaiting transplantation. To learn about our clinical trials, please call the Gastroenterology and Hepatology Clinical Studies Unit at 314-977-9400 to speak with a research coordinator.
With the surge in obesity and the escalating prevalence of Non-Alcoholic Fatty Liver Disease (NAFLD)—now affecting 24 percent of U.S. adults—nutritional counseling has become a critical component in managing gastrointestinal (GI) symptoms. Substantial evidence indicates that dietary intervention and weight loss can significantly alleviate various common GI diseases, including Crohn's Disease, Ulcerative Colitis, Celiac Disease, and Diverticular Disease. According to a exact study by the National Library of Medicine, 61% of over 70,000 surveyed individuals reported experiencing one or more GI symptoms in the past week, encompassing heartburn/reflux, abdominal pain, bloating, and diarrhea, among others. The prevalence of these issues is expected to grow over time, underscoring the importance of nutritional support. Nutrition at Allied Digestive Health Recognizing the imperative for patients to access nutritional counseling, Allied Digestive Health (ADH), a portfolio company of Assured Healthcare Partners and a regional leader in gastrointestinal care, has developed a comprehensive wellness program that seamlessly integrates nutrition counseling. The program aims to assist patients dealing with medical conditions that benefit from dietary intervention, offering disease-specific nutrition education and support for weight loss. Currently staffed by a team of dietitians throughout New Jersey with plans for further expansion, ADH represents a coordinated approach to care, providing patients with personal support from an entire team. "The connection between gastrointestinal care and nutritional counseling is evident. Through the implementation of a robust nutrition program, our objective is to empower our patients to take an active role in their health. By supporting our patients throughout their health journey, our foundation ensures a personalized approach to patient care, focusing on the alleviation of symptoms and enhancing overall digestive well-being," said Jai Mirchandani, MD, a gastroenterologist with Gastroenterologists of Ocean County, a division of Allied Digestive Health. Education and Support Participants in ADH's nutrition program are encouraged to take proactive steps toward improving their overall wellness. “As healthcare evolves, there is an increased focus on a holistic approach to care. The steps that ADH has taken towards establishing a health team comprised of gastroenterologists and dietitians foster continuous communication and coordination within an integrated network, profoundly impacting health outcomes. Beyond symptom management, nutritional counseling will bring to light the root causes of digestive issues, addressing nutritional gaps and lifestyle factors that contribute to gastrointestinal health," said Junsuke Maki, MD, a gastroenterologist with Shore Gastroenterology Associates, a division of Allied Digestive Health. Given that obesity is a major concern for many patients, contributing to increased risks of cardiovascular diseases, diabetes, inflammatory conditions, joint pain, and digestive issues, nutritional counseling becomes a vital tool for educating patients on proper nutrition and setting realistic health goals. Robin Lynch, RDN, lead dietitian at ADH, notes, "The scale never motivates patients because weight fluctuates frequently, so the goal is to focus on other health markers, such as blood glucose levels, energy levels, stamina, sleep, and anthropometric measurements, as small weight changes are made." Nutrition education and goals are tailored to meet individual needs, considering resources, mental state, social support systems, financial circumstances, and physical abilities. Melissa Stump, MS, RDN, a dietitian at ADH, adds, "One of the most challenging aspects of counseling patients about weight loss is breaking through the decades of misinformation about dieting, weight loss, and nutrition. Our program aims to combat this by promoting lasting change for our patients." Fibroscan In addition to the nutrition program, ADH now offers Fibroscan for patients. This technology assists in staging fatty liver disease, providing patients with a visual representation of their liver's condition. Given the absence of approved medications for treating NAFLD, weight loss is a critical component of improving overall patient health. ADH's treatment plan focuses on losing 5-10% of total body weight, a measure shown to Improve fatty liver disease. Despite prospective weight loss medications on the horizon, establishing lasting intake and behavior changes remains crucial. Robin Lynch, RDN, emphasizes, "Our role is to educate patients on how to make lifestyle changes to promote consistent weight loss that will motivate and empower patients to continue working toward their realistic health goals, regardless of having weight loss assistance from approved medications." Continuity of Care Allied Digestive Health is committed to providing personalized gastroenterology care through its nutrition program and the introduction of Fibroscan technology. ADH believes in a multidisciplinary approach to the treatment of GI diseases, incorporating nutrition and complementary therapies. With an ongoing focus on nutritional counseling, ADH plans to expand its wellness program to include cognitive behavioral counseling, fitness programs, support therapy, and stress management programs. Melissa Kirchner, RDN, expresses the organization's forward-looking perspective, "We are looking forward to being a resource to patients with their diagnosis through multiple approaches and approved treatments as we grow and expand our wellness program at Allied Digestive Health." About Allied Digestive Health Allied Digestive Health is a leading gastroenterology and hepatology practice with 60+ locations throughout New Jersey and New York, specializing in colon cancer screening, and the treatment of Celiac Disease, GERD, and IBD. Allied Digestive Health is committed to empowering gastroenterologists to deliver compassionate, high-quality, and comprehensive care through an unparalleled patient experience. Their team, comprised of gastroenterologists, pathologists, anesthesiologists, nurse practitioners, and physician assistants, work together to uphold the highest standards of care. Learn more at: www.allieddigestivehealth.com. About Assured Healthcare Partners® Assured Healthcare Partners® (AHP®) provides capital solutions supporting growth, consolidation, and repositioning opportunities in the healthcare services industry. Combining flexible capital with specialized research and an extensive industry network, AHP unlocks value for portfolio companies and investors. For more information about AHP, please visit www.ahpartners.com  Have you ever experienced frequent burping when dealing with acid reflux? This condition which affects your digestive health manifests when stomach acid reverses its path into the oesophagus, often accompanied by distinctive burping. We spoke to our expert Dr Aditya Shah, MBBS, MD, DM – Medical Gastroenterology, Apollo Spectra, Chennai, who explained acid reflux burping, its causes, remedies, and treatment. Causes Of Acid Reflux Burping
According to a review conducted by Neurogastroenterology and GI Motility, a healthy individual may burp up to 30 times a day on average. However, you might burp more frequently if you have acid reflux.
Remedies To Manage Acid Reflux Burping
Dr Shah listed simple remedies that you can follow to manage acid reflux burping:
Treatment for Persistent Cases
Over-The-Counter MedicinesFor milder instances of acid reflux burping, over-the-counter, antacids offer temporary relief by neutralising excess stomach acid. Medications“In more persistent cases, healthcare providers may recommend prescription medications, such as Proton Pump Inhibitors (PPIs) and H2 blockers”, said Dr Shah. These medications work to efficiently reduce stomach acid production, providing more sustained relief. Surgical ProcedureSurgical procedures, reserved for severe and resistant cases, may be considered to address underlying issues contributing to acid reflux burping. “This option is typically explored after other treatments have proven ineffective or when a structural problem, like a hiatal hernia, requires correction”, said Dr Shah. Always consult with a medical expert to determine the most suitable treatment plan based on individual circumstances. BottomlineDr Shah concluded, “While incorporating dietary adjustments and lifestyle changes can often manage the symptoms of acid reflux burping, persistent cases may necessitate medical intervention. Hence, seek guidance from a medical expert to ensure a tailored approach to treatment.” [Disclaimer: This article contains information provided by a registered healthcare expert and is for informational purposes only. We advise you to not substitute this information with medical treatment and consult your expert for medical advice.] Chasing away an infection with the right antibiotic can feel magical. Stabbing throat pain improves, coughs subside, ear aches fade. A course can save us from pneumonia and protect us during surgery. The advent of penicillin has been hailed as one of the greatest discoveries in medicine. But an antibiotic can also be a temptress. While the drugs work by killing or inhibiting the growth of bacteria, we often seek them out for runny noses and chest colds, most of which are caused by viruses. An estimated 28 percent of antibiotics prescribed to children and adults are unnecessary. When a virus like those that cause the flu or Covid is causing your symptoms, antibiotics not only don’t help, they can hurt. Swallowing an antibiotic is like carpet-bombing the trillions of microorganisms that live in the gut, killing not just the bad but the good too, said Dr. Martin Blaser, author of the book “Missing Microbes” and director of the Center for Advanced Biotechnology and Medicine at Rutgers University. Drug-resistant bacteria are already in all of us; beneficial bacteria help keep them controlled. When an antibiotic wipes out beneficial bacteria, the resistant bugs can flourish, making present and future infections harder to treat. With the overuse of antibiotics, our microbes are disappearing, a crisis with far-ranging consequences scientists don’t fully understand yet. “I think the health profession in general has systematically overestimated the value of antibiotics and underestimated the cost,” Dr. Blaser said. Antimicrobial resistance is one of the top global public health threats, according to the World Health Organization. Each year in the United States, an estimated 2.8 million antimicrobial-resistant infections occur, leading to more than 35,000 deaths. If you take a lot of antibiotics, you are at greater risk of developing an antibiotic-resistant infection and spreading it to others. That can contribute to the rise of antibiotic-resistant bacteria, sometimes referred to as superbugs. To top it off, taking antibiotics regularly may also make you more susceptible to other illnesses. Antibiotics also disrupt the good gut bacteria that are responsible for helping with metabolism, digesting food and educating the immune system. Researchers are currently studying whether this can lead to metabolic disorders, such as Type 2 diabetes, and autoimmune diseases. Research in animals suggests it does lead to chronic diseases. The data suggest this is true for humans, too, said Dr. Lauri Hicks, director of the C.D.C.’s Office of Antibiotic Stewardship, but the link between antibiotic use and different chronic diseases requires further study. In exact years, experts have been pushing for an overhaul of the way we use these medicines. “This is a mindset,” said Dr. Sara Cosgrove, professor of medicine in the division of infectious disease at Johns Hopkins University School of Medicine. “You do have to get yourself out of the traditional — to some degree, American — mindset that antibiotics are always good and don’t cause harm.” Here are a few tips on how to have an open conversation with your doctor about antibiotics. Find out if you really need an antibiotic.So your doctor suggests an antibiotic. “Say, ‘OK, doc, what are we treating here?’” recommends Dr. Jeffrey Gerber, associate professor of pediatrics and epidemiology at the Perelman School of Medicine at the University of Pennsylvania. Get a clear understanding of which bacterial infection the antibiotic is targeting. Ask if there’s a test to ensure that the medication is indicated and whether you can wait a few days to fill the prescription if you’re not improving. “A little skepticism is needed,” said Dr. Emily Spivak, an infectious diseases doctor at University of Utah Health. Also inquire which medication has the fewest side effects. Adults and children routinely go to the emergency room because of problems that arise from taking antibiotics. A broad-spectrum antibiotic, which is capable of fighting many different types of bacteria, can kill off more good bacteria and generally has more side effects, like diarrhea. This type of medication can also lead to more antibiotic resistance, although there are times when it may be the right treatment. Your physician or pharmacist can explain what kind of antibiotic is being prescribed and also tell you if a narrow-spectrum option might work. Whatever you do, don’t ask for an antibiotic: Research suggests that doctors are more likely to prescribe the medication when they perceive patients expect it. Ask for the shortest course.It was long believed that if you didn’t finish the whole course of antibiotics, the bacteria might become resistant. But evidence has emerged that the longer you take antibiotics, the more likely you are to be susceptible to another bacterial infection. “After minimizing the biological costs of antibiotics for decades, medical scientists are finding evidence that longer courses are more damaging than shorter ones,” said Dr. Blaser, who was not involved in the new research. “This will change how we approach the length of treatment in the future.” Research has also started to show that shorter courses of antibiotics for some conditions can be just as effective as longer ones. When Dr. Blaser started out in medicine, he said, physicians would usually treat a simple urinary tract infection with a two- to three-week course of antibiotics. Now it can be three days or less. The American College of Physicians recommends shorter courses of antibiotics to treat common bacterial infections, such as community-acquired pneumonia. Most cases do not require antibiotics for longer than five days. For most children, the recommended antibiotic course for a sinus infection has been cut in half, and is now 5 to 7 days; it’s similar with community-acquired pneumonia, according to the American Academy of Pediatrics. Yet some doctors still prescribe the longer courses. If that happens, Dr. Hicks recommends respectfully asking if you need to take the full course. Prolonged treatment may be needed for chronic or recurrent infections; a specialist can help make the determination, Dr. Blaser said. Some experts suggest asking whether you can stop your antibiotics if you’re feeling better. “Some patients are going to have rocket immune systems, and be young and healthy, and they might be better after just a couple days,” said Erin McCreary, a pharmacist and director of infectious diseases improvement and clinical research innovation at UPMC. Rethink probiotics.Often doctors will recommend taking a probiotic in conjunction with an antibiotic, in order to ease some of the associated diarrhea and with the idea that it can help restore the microbiome’s array of good bacteria. But Dr. Blaser said the jury is still out: Some findings suggest that probiotics may possibly prolong the time it takes for the microbiome to return to its pre-treatment state. There’s some evidence that probiotics may help prevent antibiotic-associated diarrhea, though it’s not conclusive, said Hye-Sook Kim, a program director who oversees microbiome and probiotics research at the National Center for Complementary and Integrative Health. Probiotics may reduce the risk of developing the life-threatening infection Clostridioides difficile, which can cause severe diarrhea and inflammation of the colon, called colitis. It’s usually caused by exposure to antibiotics; those who take them more frequently are at greater risk. For the majority of people, Dr. Spivak said probiotics are “fine to take, I just can’t certain it’ll make any difference.” If you are going to take them, you might do so after finishing your medication. “Practically speaking, it’s spitting in the wind to take them simultaneously,” since an antibiotic can kill the good bugs in a probiotic, said Dr. Neil Stollman, a gastroenterologist at Alta Bates Summit Medical Center in Oakland, Calif., and a fellow of the American College of Gastroenterology. Of course, even the experts who are critical of antibiotic overuse take the medicine sometimes, when really needed. Dr. Blaser himself took a full course after noticing a huge bull’s-eye on his torso, the telltale mark of Lyme disease. And Dr. Cosgrove did, too, after her black cat, Angus, scratched her. “The redness was crawling up my arm,” she said. “Antibiotics were definitely indicated.” A short course quickly cleared it up. Several years later, neither doctor has taken antibiotics since. IRVING, Texas, Jan. 3, 2024 /PRNewswire/ -- NorthStar Anesthesia, an industry leader in anesthesia care, has expanded its high-quality anesthesia services to Portneuf Health in Pocatello, Idaho.
Portneuf provides high quality healthcare services throughout Southeast Idaho. Portneuf turned to NorthStar Anesthesia to support the modernization and scale of its anesthesia services to accommodate growing case volumes and better serve the Pocatello community and region. NorthStar is serving Portneuf Medical Center, the Rocky Mountain Surgery Center and Portneuf Gastroenterology and Endoscopy Center, which collectively include a neonatal intensive care unit, a full suite of cardiac care, imaging, and primary and specialty care. "Our partnership with NorthStar Anesthesia will help us to better serve our community and the region, with quality resources and first-class reputation for high-quality patient care," said Jordan Herget, President and CEO of Portneuf Health. "Investing in our anesthesia practice is important to facilitating our long-term, sustainable growth, enabling us to provide the highest quality of care to an ever-growing number of patients." NorthStar retained 100% of Portneuf's current CRNAs and anesthesiologists, which is a testament to the alignment between NorthStar's values and the strong existing culture among the anesthesiology team at Portneuf. "We are excited for NorthStar's first venture into Idaho and look forward to working with the team at Portneuf, as well as expanding our collaboration with their parent company Ardent Health Services," said NorthStar Anesthesia CEO Adam Spiegel. "This transition is an investment into an exceptional set of facilities that will benefit patients across the entire region of Southeast Idaho." NorthStar's partnership with Portneuf began on December 1, 2023. About NorthStar Anesthesia About Portneuf Medical Center The governance of Portneuf Medical Center is split 50/50 between Portneuf Health Trust and the parent company Ardent Health Services As a major employer in Pocatello, we have 1,600 well-qualified employees and we continue to grow. Media Contact:
View original content to get multimedia:https://www.prnewswire.com/news-releases/northstar-anesthesia-to-provide-anesthesiology-services-for-portneuf-health-302025435.html SOURCE NorthStar Anesthesia | ||||||||
CGRN course outline | CGRN PDF Download | CGRN study tips | CGRN plan | CGRN action | CGRN PDF Download | CGRN test plan | CGRN resources | CGRN test contents | CGRN study tips | | ||||||||
Killexams test Simulator Killexams Questions and Answers Killexams Exams List Search Exams |